7 2 - 雙語字幕
Hi welcome back to part two of our randomized control trials lecture.
So in the first part we looked at selection issues and how they relate to how they
need to be considered with regards to randomized control trials.
But in this part of the lecture we're looking at measurement issues.
Now, the thing to consider with measurement, particularly for randomized control trials, is blinding.
Now, in a randomized control trial, ideally we want as many people as possible to be blinded.
We participants.
the study staff,
the investigators,
the outcome assessors,
even the statisticians and people that are writing up the results to become,
to be blinded to the intervention or control group that the participants are in.
And even from the point of the statistician,
you might be thinking, how is it possible they've got to analyze the results and write up the results?
But it is possible in that we might allocate them or the data is provided to the statistician
in terms of group A and group B.
So they analyze it with regards to, yep, group A had the average result, had these results and group B had those results.
But they don't know what group A was, was it the intervention group or was it the control group?
So only after the results are written and the papers written is the code broken and then everyone becomes unblinded to the results.
Now there is good evidence showing that blinded trials provide different results than unblinded trials.
In that I guess unblinded trials are more likely to give a biased result compared to blinded trials.
Now these studies are conducted similar to the charmer's paper that I was talking about earlier with regurgers.
So, these studies looking at unblinded compared to blinded studies showed that there was some difference in the results obtained.
Now, how does blinding minimise bison studies?
It does so in three different ways.
It at preventing contamination, co-intervention and bison.
So contamination is just when those that are in the placebo group go off on their own and
obtain the intervention that's being administered in the trial from other means so they might
go to another healthcare provider to obtain the intervention being evaluated and still
remain
Co-intervention is when those in the placebo group head out and although they
may obtain other treatment not the treatment that's being investigated in the trial but an alternative treatment that might be impacting upon their outcome.
And-driven reporting as you can appreciate is just having an outcome that's reported in a biased fashion.
they know which group they're in.
Now, just because a study starts off as being blinded, it doesn't mean that participants remain blinded during the study.
And most people at some point during the study,
if you ask them, will have developed a belief as to which treatment group that they were assigned to.
And this belief whether it be correct or incorrect may result in them obtaining, becoming contaminated, obtaining co-interventions or event bias event reporting.
So, how can we tell with a blinding light?
Well, we actually probably can't tell whether a study was blinded for the duration.
All that we can do as people that are using randomized controlled trials in our evidence
decision making is check whether the investigators made every attempt possible to blind participants during the study.
Now, there are lots of different types of biases that you'll hear whilst you're reading, whether
they're reported in the textbook or in other articles that you're reading, and we're not really focusing on it.
We don't need to worry about naming those particular biases, but I am going to particularly mention the two terms performance bias and ascertainment bias.
as they're both related to blinding.
So performance bias is just relating to how people perform during the study,
whether they do things differently because of which group that they've been allocated to.
For example, someone in the placebo group might act differently to someone.
group, because those in the placebo group, as I said, might go out and seek other treatments,
whereas those in the active group may not, which is the contamination or common dimension.
But also, we need to consider the people in the active group might behave differently.
So people in the active group might imagine or believe that they've developed a side effect
treatment and therefore they go off and get this side effect managed or they change their behaviors they might withdraw from the trial.
They might just behave differently than those in the placebo group because they
know that they're not getting the treatment so they know that this particular symptom isn't a side effect so they don't worry about it.
And that's an example of performance bias.
An ascertainment bias is really describing how hard outcome assessors go to determine whether or not an outcome is there.
So it may be as simple as, for example, if the outcome is a subjective measure or has some subjectivity to it.
that if I'm the outcome assessor and I know that an individual was in the intervention group, I might look a little bit differently.
I might look a little bit harder to try and classify these symptoms as the outcome.
When if they've been in the placebo group, I may not consider that being the outcome.
So it's just me behaving differently.
based on my understanding of what treatment group they're in and that's an example of acetaminate bias.
Now what did the waschop study do with regards to blinding and their measurement?
So here is an extract from the It says here that the potential end points,
so what the outcome was, were reviewed and classified according to predefined criteria.
So that's great in terms that it was predefined before the study was developed and conducted.
They a set criteria and they knew exactly what the outcome was going to be and how the outcome was going to be assessed.
It's also great that they used a committee and it wasn't just one individual person and it was a consensus.
And then down the bottom it's got a little bit about the blinding,
except for the trial statistician and his assistant, all trial personnel remain unaware of the subject's treatment assignments throughout the study.
So, that's a good evidence as good as we can see that everyone within the trial
was blinded and attempts to minimize bias in terms of outcome reporting was employed.
And here's another example from another trial looking at TPA which is a,
a clot-busting And here we are looking at the different outcome measures and showing that they were actually quite well defined and blinded.
So here in this particular study, they had a particular index that was self-reported.
And outcome was assessed at 24 hours and at three months by examiners who had not been present at the baseline.
or during treatment.
So would imply that they were blinded to which treatment group they were in.
So if we just pause here for a moment and think about what we've already discussed.
So we've gone through a little bit about selection and measurement within randomized control trials.
Now in selection of randomized control trials, the unique feature that we need to really think about is the randomization process.
making, which is considering the randomisation list and how it was generated, as well as allocation
We need to also consider follow-up whether everyone that was followed up and if they weren't followed up,
what happened with those people or how were those outcomes dealt with.
And were they,
did they take an intended So, there are the typical important features, I guess, that we're looking for within a randomized control trial.
Now, with regard to measurement, as we've all studied designs, I think we really need
to think about how the outcome was measured, but in particular circumstances of the randomized control trial, be one of the considered blindfolders.
blinding?
Who was blinded?
Who wasn't blinded?
And what's the outcome of this blinding or this lack of blinding?
Now you need to bear in mind,
and the allocation concealment and blinding are two different things,
although they might seem to be related They're very different and they need to be considered separately.
Allocation concealment is a selection issue, whereas fundamentally blinding is a measurement issue.
And remember, it is possible to have a study that's got proper allocation concealment, but is not blinded.
Likewise, we can have a study that does not employ allocation concealment but is blinded.
So there are two different elements and need to be discussed separately and considered separately.
Now, with regards to randomized control trials,
there are strict rules and protocols
that should be followed in here too when designing And you'll find most of those listed within the Consort statement.
The Consort is a great place to go to with regard to randomized control trials.
The Consort has actually been extended now to look at different types of trials,
but it was, it was sort of the, I guess, the gold standard of how to design and report randomized control trials.
And one part of the consult statement is a newly developed, developed back in 2010 in the updated version of the consult statement.
Is this a flow chart?
Now, the other flowcharts that we've looked at, and flowcharts that we actually use
for a lot of our tutorials,
ours are slightly different drawings and designs in that our follow-up groups are often off to the side,
and in my mind that provides a little bit more of a logical sense as the flow of people through the study,
as we have here, the excluded people off to the side.
However, this is the consult recommendation and you'll see many flow charts drawn like this
showing the selection of people and the flow of people through the trial.
But irrespective of how it's drawn, I would imagine every RCT has a flow chart similar to this indicating the flow of people.
Again, let's move on to the results.
So what do we look for when we're evaluating the results or reading and considering the results of a randomized control trial?
So headed back to our WASC-COB study, they've got some results in their abstract here.
Talking about, if you can see here, I'll see you in little bit.
And 174 in the Provost Dutton group with a relative reduction in risk with Provost Dutton of 31% with a particular confidence interval.
And then they talk about here about a 22% reduction in the risk of death in the Provost Dutton group.
So that's there in the abstract.
So we'll have a look at the results.
and see what they've got.
So here's the table,
and here they're reporting relative risk, and in this case, given that the intervention was a benefit, they're reporting the reduction in relative risk.
But they're not calling it that,
they're just calling it a in the risk So in terms of the outcomes of non-fatal myocardial infarction or death from coronary heart
disease So this is in all the people who had the event all 248 of them yeah 7.9%
of them 7.9%
in the placebo group, and 154, or.5% of them in the probestatin group, experienced the outcome of a nonfatal myocardial infarction or death.
So the incidence of 7.9 and an incidence of 5.5 gives us roughly a relative risk of 0.7,
which gives us a relative risk reduction of 31%, which is where that 31 comes from.
So if you look at non-fatal or death,
you get a similar and remove the not the remove sorry and remove the silent myocardial
infarctions you get roughly the same results similar not exactly the same but similar
enough And if we just look at the non-fatal myocardial infarctions, again, it's similar with the relative risk reduction of 31%.
And if you look at deaths from coronary heart disease,
and it's p-value, most of you will know that p-value of greater than 0.05 is not statistically significant.
So some people won't pay any attention to these results down here, although as they're not significant.
But it's actually the estimate of risk, the risk reduction is somewhat similar.
So although it's not significant, it's providing a similar set of results.
So how come these top three here is significant whereas our last one isn't?
And I think the answer comes down to...
the precision of our estimates, and we can see here, although in both groups, we the same number of people, 3,293...
Sorry, not in both groups.
In all the outcomes,
I guess, we had the same denominator of 3,293, but in the case of death, we only had 52 and 38 of them.
So our numerator is somewhat smaller than the other example or the outcomes.
So our confidence intervals are a lot wider given the smaller event numbers.
Now I'm just mentioning this just because,
but even though it's not statistically significant,
you shouldn't just ignore you should look at the estimate of effect and see if it's consistent with the other things.
And we would say here that yes, it is quite consistent with the other results.
And we could argue that perhaps the sample size has been bigger and therefore we would have seen more events of death,
we might have obtained the results.
Now, this is the last sort of main thing we wanted to focus on this week.
Now, in terms of generalizability, it's generally accepted that if you have something biological, it should be generalizable from one population to another.
So results that we obtain in one population should be generalizable to one
But it's not always the case because there might be a different genetic make up that's important, but generally it's generalizable.
However, there may be situations where you don't necessarily want to make the same decision from one population to another population.
So looking here, we have the results and we would say that there's a 7% incidence in the placenta.
So, that's the background incidence and 4.7% incidence in the treated group, so that's our Provostatin group.
So, if you calculated the relative risk from the previous incidence numbers, you'd end up with a relative risk of 0.67 on a relative risk reduction of 33%.
So you also get an absolute risk reduction of 2.3%,
and so that's the absolute decrease in the incidence of having a heart attack or dying from coronary heart disease with 2.3%.
And the number needed to treat it would be in this category.
Which means we would have to treat 44 people to stop one person from having a heart
attack or die from heart disease in this particular population.
But say we had a population where the baseline rate is much higher.
Previously was 7%, but here it's 20% in a different community.
So, we'd have roughly the same relative risk and relative risk reduction, but the absolute
risk reduction is much higher, it's nearly 7% and the number needed to treat is much lower.
So you'd have to treat a much,
you could treat a much smaller number of people to obtain the same outcome,
only treating 16 people to have one person preventing the event from occurring.
So in this situation it's more efficient and much more cost effective to have the treatment.
But what if we were to go to another community where we had a much lower baseline event rate,
where we had an incidence rate in our placebo group of about 2 percent?
We still have the same relative risk and relative risk reduction of 33 percent,
but the absolute risk reduction is so much less, less than 1 percent.
And now our number needed to treat is 152 people.
So the thing that's portable between populations is the relative risk.
So the relative risk will apply from one population to the other population irrespective of their baseline risk.
What does change is the absolute risk reduction.
Okay, our absolute risk reduction depends on our baseline risk.
So you might end up making a different decision in one population compared to another population,
even though the drug works just as effectively in terms of the relative extent to which it decreases the risk.
And finally, where do we go to find randomized controlled trials?
Well, here is a medline search through over that was conducted when we were interested in looking at provostatin to prevent coronary disease
and of those 59 results that were obtained WASTCOM study was one of those papers.
So the first point of call,
I think, for most people in terms of looking for randomized controlled trial evidence, if we happen to have access to MEDLINE.
PubMed is a free, similar search engine, so everyone should have access to PubMed as well.
You can also go to the Cochrane Library.
Now we'll talk more about the Cochrane Library in a few weeks or Cochrane in general in a few weeks.
But the Cochrane is one place you could go if you're looking for clinical trial evidence.
Now, there's also the Australian New Zealand clinical trials registry, and that every clinical trial that's now been conducted needs to be registered.
So if we were based here in Australia and we're wanting some evidence that was probably generated here in Australia or New Zealand,
you might want to head here.
Now this will include trials that have been conducted that haven't yet been published.
which is a great source of information.
Now there's also a similar registry in America, the clinicaltrials.gov website that will again register all clinical trials.
Now this is a specific cancer clinical trials register.
So again,
if you're looking,
it's a useful place to go if you're looking for some trials on that are concerning with cancer that may or may not have been published yet.
Now these trial registry platforms are a requirement of every sort of journal to now publish.
If you want to have your randomized controlled trials published, you need to have readhead them registered.
In a particular platform, it doesn't matter which platform, as long as it's one of the recognised trial platforms.
And World Health Organisation also has a list of many other registry platforms around the world that might be worth looking at.
Okay, and so that's it, that's the end of our randomized controlled trials lecture.
So having listened to this lecture now and then at the end of the tutorials and the quizzes,
you'll have some understanding of why randomized controlled trials are so important and how to critically appraise them and a couple of the key features.
解鎖更多功能
安裝 Trancy 擴展,可以解鎖更多功能,包括AI字幕、AI單詞釋義、AI語法分析、AI口語等
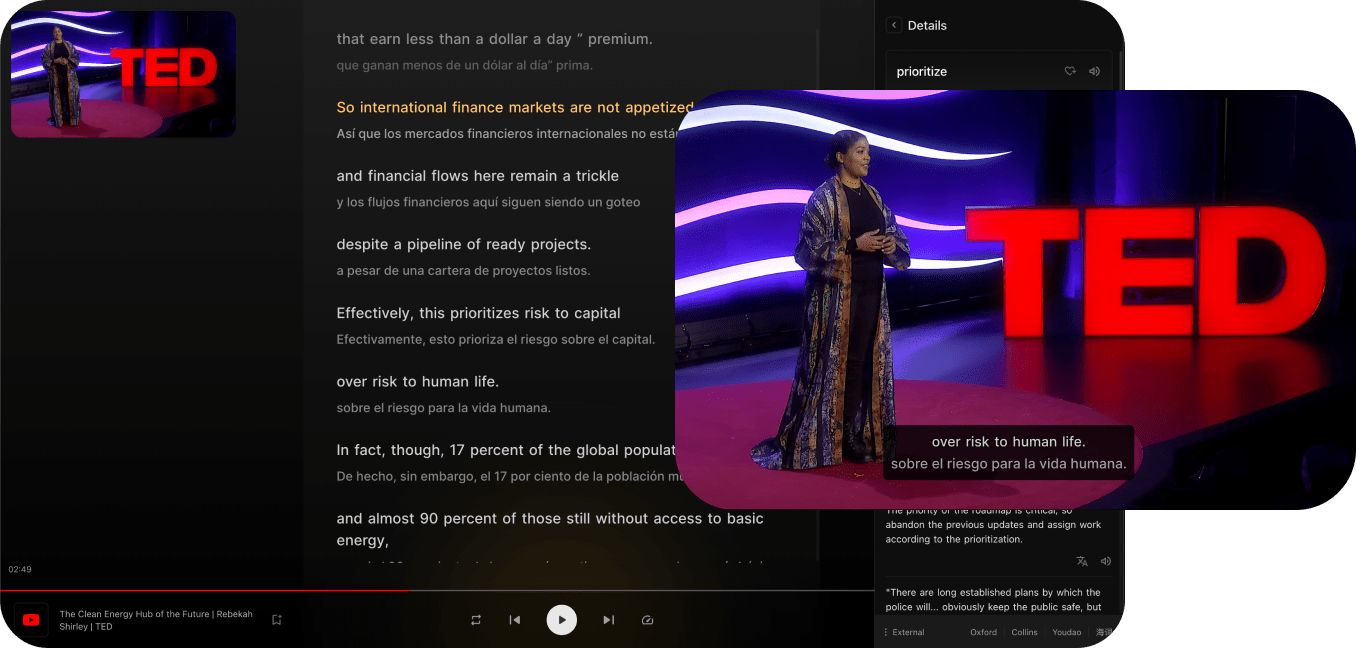
兼容主流視頻平台
Trancy 不僅提供對 YouTube、Netflix、Udemy、Disney+、TED、edX、Kehan、Coursera 等平台的雙語字幕支持,還能實現對普通網頁的 AI 劃詞/劃句翻譯、全文沉浸翻譯等功能,真正的語言學習全能助手。
支持全平臺瀏覽器
Trancy 支持全平臺使用,包括iOS Safari瀏覽器擴展
多種觀影模式
支持劇場、閱讀、混合等多種觀影模式,全方位雙語體驗
多種練習模式
支持句子精聽、口語測評、選擇填空、默寫等多種練習方式
AI 視頻總結
使用 OpenAI 對視頻總結,快速視頻概要,掌握關鍵內容
AI 字幕
只需3-5分鐘,即可生成 YouTube AI 字幕,精準且快速
AI 單詞釋義
輕點字幕中的單詞,即可查詢釋義,並有AI釋義賦能
AI 語法分析
對句子進行語法分析,快速理解句子含義,掌握難點語法
更多網頁功能
Trancy 支持視頻雙語字幕同時,還可提供網頁的單詞翻譯和全文翻譯功能